Last month we published our latest report, Research in global health emergencies: ethical issues – the result of an in-depth two-year inquiry by an international working group with input from researchers, policy makers, practitioners and research participants in more than 30 countries across the globe. In response to the urgent need for a rigorous evidence base to support effective emergency response, the inquiry aimed to identify ways in which research could be conducted ethically even in these most difficult and distressing circumstances.
A call for action, published alongside the report and supported by leading research institutions, funders and humanitarian organisations in Europe, Africa, and Latin and North America, highlights key recommendations and responsibilities. These include the need for:
- investment in community engagement mechanisms to ensure that the voices of those directly affected by emergencies are heard in the development and conduct of research;
- carefully planned partnerships between researchers and those responsible for emergency response to ensure that research is not taking place in the absence of basic health services;
- equitable collaborations between research organisations, particularly between external research institutions and their local partners in high- and low-income settings; and
- a focus on the continuing vital importance of emergency planning and preparedness.
The report covers a wide range of emergencies, from epidemics (Ebola, Zika, Lassa fever and many others) to human-made and natural disasters. Given the timing, there is, however, one striking absence – not one mention of the novel coronavirus, now named COVID-19, that first emerged from an as-yet-unknown animal reservoir in December 2019 and is now dominating both media and political debate worldwide. In the nature of such substantial consensus-building projects, there was a short time lag – no more than a few weeks – between the signing off of the final text of our report, and the delivery of the printed copies ready to launch. It was at precisely that time that the first reports of a novel virus started to emerge from China …
The challenge of COVID-19
So what relevance has our report to the enormous challenges being posed to health systems and governments the world over by COVID-19? Unsurprisingly, quite a lot. Indeed the sudden emergence of a new disease might be considered to illustrate some of the central tenets of the report – that new health threats can at any time develop into emergencies; that no country, rich or poor, is exempt; that research has a key role to play in effective response; and that all countries have an ethical obligation, founded in solidarity, to prepare themselves for such eventualities, and to support others in so doing.
COVID-19 is a prime example of ‘Disease X’ – the unknown health threat included in the current list of priority diseases for research as part of the WHO’s Research & Development Blueprint. Its emergence illustrates vividly the fundamental role of international collaborative research in even beginning to respond effectively to such a health threat. The speedy genetic sequencing of strains of the virus from early patients, for example, has permitted accurate diagnosis of those affected, and provided the crucial starting point for the development of possible treatments and vaccines. Despite this early research success (the equally rapid sharing of those genomes with WHO and researchers around the world being described as ‘remarkable’ by researchers), the list of unknowns nevertheless remains daunting. Three of our working group members were amongst the 300 international experts and research funders convened by WHO on 11-12 February to help identify and prioritise essential research questions. Among many others, these include better understanding of how the disease is transmitted; the creation of speedier diagnostic tools; the development of candidate vaccines and treatments; and the full integration of social science research in outbreak response. People’s attitudes, beliefs and behaviours play a critical role in how diseases spread. Research that engages seriously with these social aspects of epidemic transmission and control is going to be essential both in gaining the necessary understanding, and in ensuring that response measures are culturally sensitive and appropriate. (See, for example, this thought-provoking blog on why simply banning ‘wet markets’ may not be the best approach.)
Provisional findings of the WHO expert forum draw explicitly on our report to conclude that key ethical issues can be anticipated; that useful and authoritative ethical guidance documents are in place to support researchers; and that ethics and ethics oversight are absolutely not a barrier to effective research. The specific ethical issues identified for researchers to address as they develop COVID-19 research plans are referenced directly to our work: community engagement, data sharing and transparency, priority setting, and healthcare worker support.
Research guided by an ethical compass
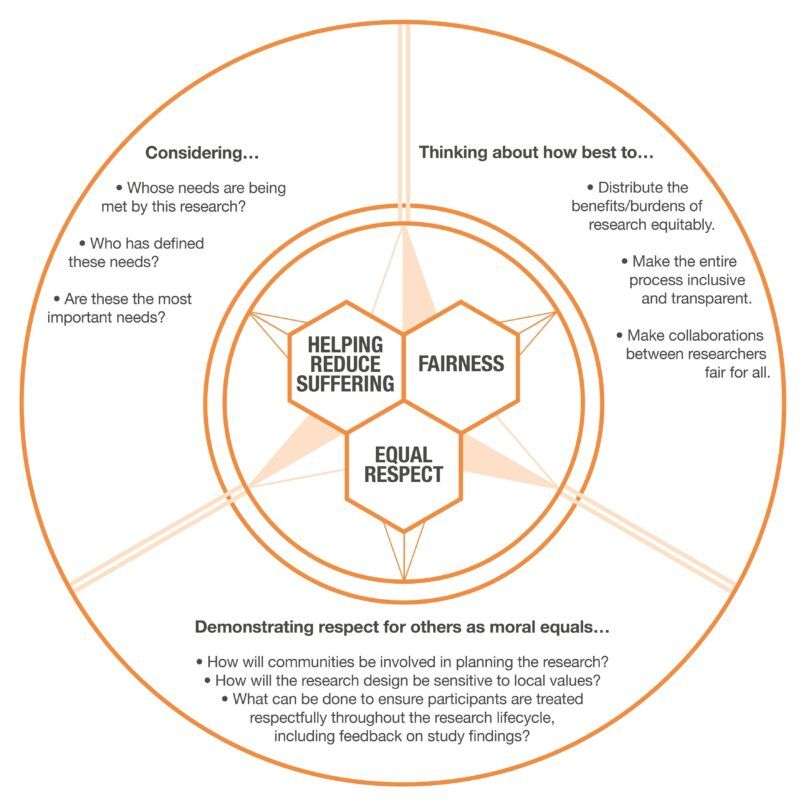
All the recommendations in our report are underpinned by three core ethical values that together make up an ‘ethical compass’: helping reduce suffering; demonstrating respect for others as moral equals (‘equal respect’); and fairness.
Helping reduce suffering provides the primary justification for research to take place at all in such cases. It provides both a constraint on what research should be considered (never research for research’s sake) and guidance on what research should be prioritised (recognising that research demands time and energy by others, and that allowing one study might crowd out another, potentially more valuable). The expert plenary meeting hosted by WHO provides a welcome example of an inclusive and international approach to the setting of research priorities for responding to COVID-19. The next challenge will be the way that those priorities will be translated by researchers and funders into concrete research plans, and how they will involve affected communities in that developmental process (of which, more below).
Questions of fairness arise throughout the research endeavour, and between many different research actors – from considerations of how benefits and burdens are distributed among research participants, to ensuring that collaborations between institutions in more and less well-resourced settings are as equitable as possible in the circumstances.
Demonstrating respect for others as moral equals underpins many of the core recommendations of our report, including those ethical priorities for the current outbreak identified by the WHO forum. Meaningful community engagement, based on respectful relationships between researchers and communities (themselves often highly diverse) is essential for research to be conducted ethically ‘with’, not ‘on’ those who are living through the emergency. Equal respect similarly underpins our emphasis on effective partnerships between research and response agencies, arguing that it is profoundly unethical for people to be approached to take part in research (however potentially valuable) if their own basic healthcare needs are not being addressed as part of the response effort. While researchers cannot themselves be directly responsible for meeting such needs, they must be confident that they know how to refer on to those who are (and that those services are in place). Equal respect also reminds us of the importance of the welfare of front-line research and healthcare workers themselves, and the responsibilities of their employers and funders to make sure that their needs are not overlooked.
Ethical research in context
These three issues, of community engagement, access to basic care, and frontline worker welfare all emerged very powerfully in recent (and – let us not forget – ongoing) Ebola outbreaks. At first glance, the challenges of COVID-19 might seem very different, emerging in a vast country with relatively developed health services, good research capacity, and a political system that allows for extraordinarily speedy building of new health facilities and deployment of health and military personnel wherever they are most required. But the longer the outbreak continues, the more clearly the parallels emerge with recent outbreaks in countries with much weaker health and research systems. The immense pressure on the health system in China is evidenced through accounts of seriously-ill people unable to access a hospital bed and of overburdened health care professionals working long hours with inadequate protective clothing, unable even to pause to eat or use the toilet. While the Chinese authorities have been praised for their ready sharing of information with international authorities, significant concerns are emerging over the degree of openness and accuracy of public communication within China, exacerbated by the news of the death of Li Wenliang, one of the first doctors to identify that a new virus had emerged, who had been visited by the police for ‘spreading rumours’.
The reality of life both in the crowded hospitals in Wuhan, and in the areas (both inside and now increasingly outside China) subject to quarantine arrangements, reminds us vividly of the importance of keeping the equal moral worth of every individual in view when making decisions for the public good. One of our working group members, Julian Sheather, in an thought-provoking blog on the ethical implications of quarantine, highlights how decisions to limit individual rights create new duties of reciprocity on the part of the state: duties to ensure people’s basic needs are being met, that their losses are compensated, and that they have access to accurate and up-to-date information. In short, that, despite the exigencies of their situation, they feel treated with respect.
In the research context, yet more is demanded in terms of information: meaningful community engagement goes beyond clear communication about research plans (although that is certainly a necessary minimum) and at its best takes the form of respectful relationships that facilitate ongoing dialogue, enabling community concerns and experiences to help shape and inform research questions, study design, and the conduct of the research from start to finish. Such engagement will be crucial in informing locally acceptable study designs for both vaccine and intervention studies as these develop – and in ensuring that communities have sufficient well-founded trust in the studies for researchers to be able to recruit sufficient participants and produce meaningful results. In a climate of fear and distress, issues of who gets access first to novel vaccines and interventions, and whether such decisions are seen to be taken fairly, will be critical in determining whether or not research can go ahead on the basis of community trust and acceptability.
Predictability, preparedness – and the need for solidarity
Finally, it is worth returning to the question of preparedness. Emergencies are, at least to a degree, predictable, and what is needed to prepare for them is increasingly well-established. What is, however, sadly often lacking is the political will to act before it is too late. The 2019 Global Health Security Index deemed no country in the world fully ready to respond to biological threats. As the Global Preparedness Monitoring Board commented in its first annual report last October: “Preparedness is hampered by the lack of continued political will at all levels. Although national leaders respond to health crises when fear and panic grow strong enough, most countries do not devote the consistent energy and resources needed to keep outbreaks from escalating into disasters.”
This lack of political will and solidarity is also true in terms of support from richer countries to poorer to support the latter’s preparedness. What turns a health threat into a full-blown emergency is often neglect. Neglect of the economic, health and other needs of marginalised or overlooked populations means that those who are most vulnerable through poverty, lack of access to health care or lack of political voice are disproportionately the most affected by health emergencies. In particular, lack of basic health services can hinder early recognition of, and hence effective response to, emerging threats. It is no surprise that the WHO Director-General’s declaration on 30 January that the COVID-19 outbreak constitutes a Public Health Emergency of International Concern was made specifically with reference to “the potential for the virus to spread to countries with weaker health systems, and which are ill-prepared to deal with it”. (See, for example, modelling published in the Lancet last week regarding the implications for Africa, despite considerable efforts by many countries on the continent to step up their preparedness to detect and cope with COVID-19.)
WHO Director-General, Dr Tedros Adhanom Ghebreyesus, has not been shy in linking emergency preparedness with progress on Universal Health Coverage. Nor has he hesitated to highlight how lack of funding for the WHO limits its abilities to plan even a month ahead. In the context of the ongoing Ebola outbreak in the DRC (which remains a public health emergency of international concern even though media interest has evaporated in face of the new threats posed by COVID-19), Dr Tedros tweeted on 21 February: “Even though new #Ebola cases in #DRC have thankfully declined, we remain in full response mode. But there is a lack of funding for @WHO activities beyond February. We still need support from the international community to end this outbreak for good”.
How many more global health emergencies will it take to achieve a fundamental shift from ‘panic-mode’ funding, too little, too late, to the sustained international investment required to support every country in the world to develop the kind of health systems that could help keep us all safe?